Community Member
Hepatitis C: Test, Treat, Cure
For tribal community members about recognizing the symptoms of hepatitis C and the importance of getting treatment.
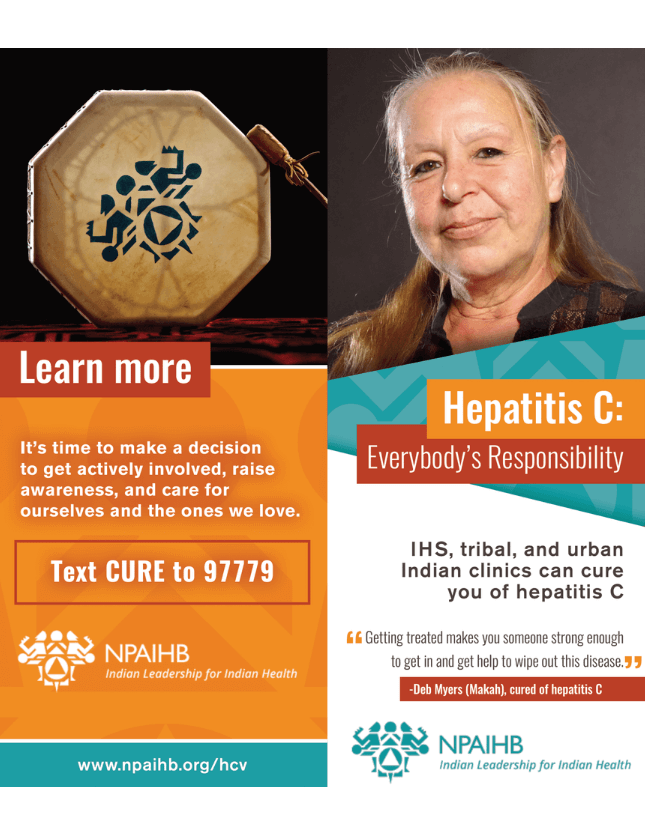
Hepatitis C is Everyone’s Responsibility
PSA for American Indian and Alaska Native community members about how hep C is everyone’s responsibility.
Health Provider
Want tips for developing your own HCV micro-elimination program?
Free service to help I/T/U providers treat complex medical conditions.
Want to expand screening, management, and pre-treatment of HCV?
IHS, Tribal and Urban Clinics are Curing Hepatitis C
Providers can make a difference in patients’ lives through diagnosing hep C early. Learn more about screening and offering patients effective- potentially life-saving – treatment.
Print Materials:
-
Hepatitis C: It’s Everyone’s Responsibility
-
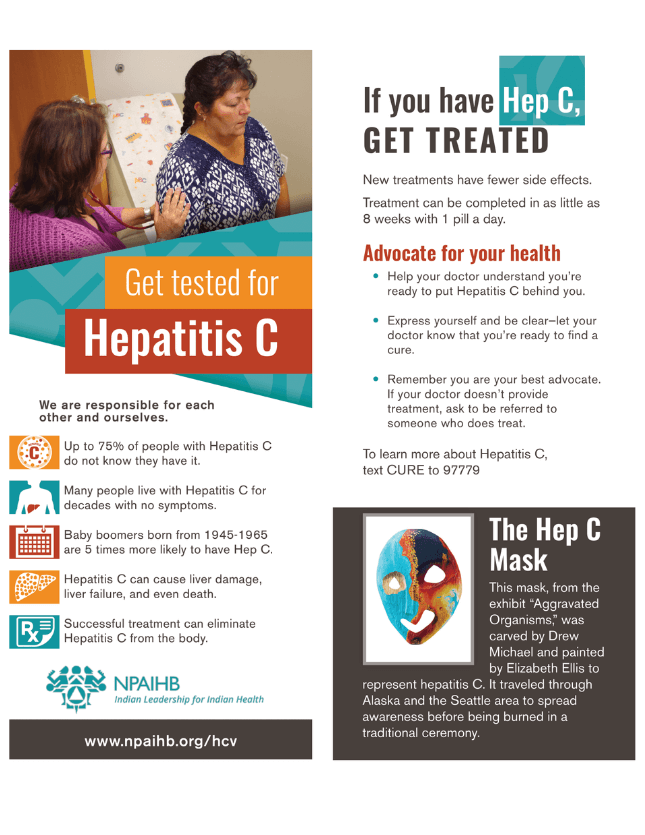
Get Tested for Hepatitis C
-
Hepatitis C: Test, Treat, Cure
-
Hepatitis C: Why Baby Boomers Should Get Tested
Text Message Campaign:
HCV Text Message Campaign Card
To be posted in clinical settings to encourage patients to text ‘HCV’ to 97779 to receive information about preventing, treating, and recovering from Hepatitis C.
Short Films:
Hepatitis C: Test, Treat, Cure
For tribal community members about recognizing the symptoms of hepatitis C and the importance of getting treatment.
Hepatitis C Is Everyone’s Responsibility
PSA for American Indian and Alaska Native community members about how hep C is everyone’s responsibility.
Audio PSAs:
Hepatitis C Audio PSA – Female
Hepatitis C Audio PSA – Male
Print Materials:
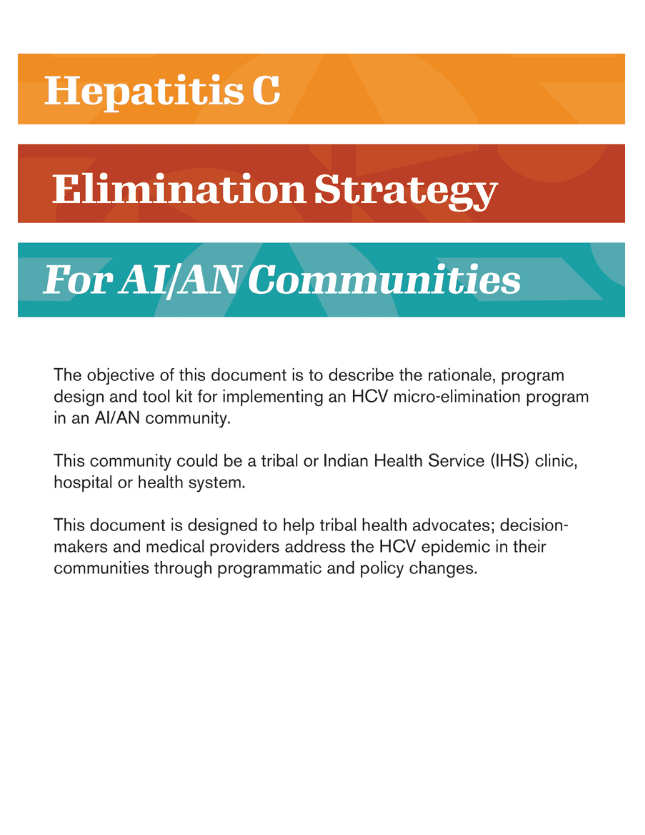
Hepatitis C Elimination Strategy for AI/AN Communities
Comprehensive guide for healthcare providers and tribal decision-makers seeking to develop a community-tailored HCV micro-elimination program.
Hepatitis C: It’s Everyone’s Responsibility – For Clinicians
Provides essential facts about HCV and tips for talking to patients about HCV testing and treatment.
Are You Screening for Hep C?
Fortunately, hep C is curable for most, but it is up to clinicians to screen and appropriately diagnose patients. Check out this tip card for more info.
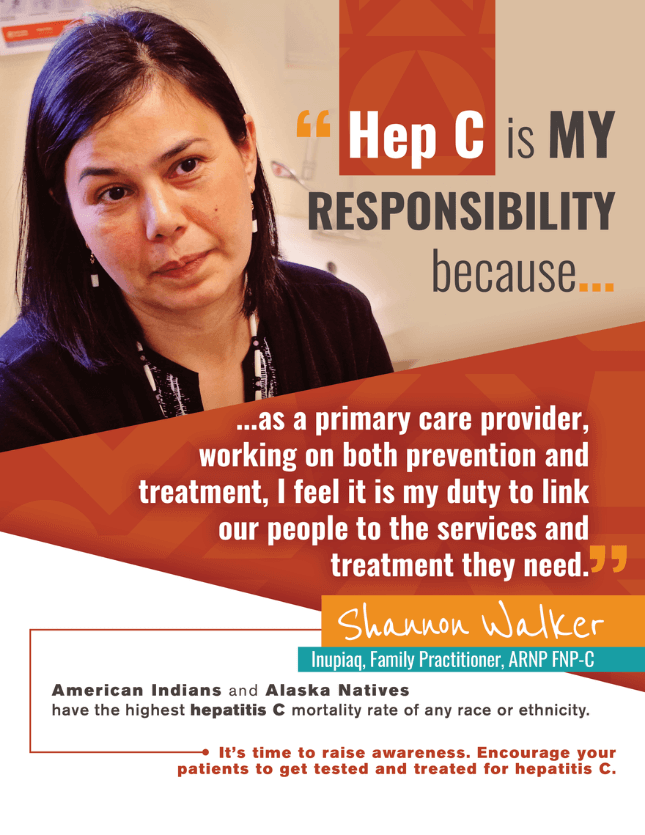
Hep C is My Responsibility Campaign Posters
In 2017, the Northwest Portland Area Indian Health Board launched a campaign to encourage clinicians at IHS, tribal, and urban clinics to screen, diagnose, and treat patients with HCV; these posters for clinicians are perfect for treatment rooms.
Short Films:
IHS, Tribal, and Urban Indian Clinics are Curing Hepatitis C
Providers can make a difference in patients’ lives through diagnosing hep C early. Learn more about screening and offering patients effective- potentially life-saving – treatment.
Guide to Developing and Managing Syringe Access Programs
Comprehensive manual for starting and managing syringe access programs; guidance offered in several areas including: Planning and Design, Operational Issues, Organizational Issues, External Issues and Population-Specific Considerations.
Compassion, Action, and Healing: Working with Injection Drug Users in Native Communities
Important information relevant to people who inject drugs and those who work with this population.
Getting Off Right: A Safety Manual for Injection Drug Users
Easy-to-read survival guide for people who inject drugs (PWID); a compilation of medical facts, injection techniques, and strategies to keep PWID healthier and safer.
North American Syringe Exchange Network
Organization that offers useful information about starting and supplying syringe exchange programs.
Indian Country ECHO – Technical Assistance and Capacity Building
Free service designed to optimize I/T/U clinical policies, enhance care delivery for patients, and build community capacity to prevent and treat complex medical conditions, including hepatitis C.
Tribal Leader
Want tips for developing your own HCV micro-elimination program?
Free service to help I/T/U providers treat complex medical conditions.
Want to expand screening, management, and pre-treatment of HCV?
IHS, Tribal and Urban Clinics are Curing Hepatitis C
Providers can make a difference in patients’ lives through diagnosing hep C early. Learn more about screening and offering patients effective- potentially life-saving – treatment.
Indian Country ECHO’s HCV Clinical Resources
Up-to-date list of clinical resources for preventing and treating HCV.
HCV Cost Calculator
Use this treatment calculator to discover the costs of treating HCV based on your community needs.
Guide to Developing and Managing Syringe Access Programs
Comprehensive manual for starting and managing syringe access programs; guidance offered in several areas including: Planning and Design, Operational Issues, Organizational Issues, External Issues and Population-Specific Considerations.
Compassion, Action, and Healing: Working with Injection Drug Users in Native Communities
Important information relevant to people who inject drugs and those who work with this population.
Getting Off Right: A Safety Manual for Injection Drug Users
Easy-to-read survival guide for people who inject drugs (PWID); a compilation of medical facts, injection techniques, and strategies to keep PWID healthier and safer.
North American Syringe Exchange Network
Organization that offers useful information about starting and supplying syringe exchange programs.
Hepatitis C Elimination Strategy for AI/AN Communities
Comprehensive guide for healthcare providers and tribal decision-makers seeking to develop a community-tailored HCV micro-elimination program.
Indian Country ECHO
Free service for I/T/U clinicians and programs to enhance care delivery for patients with complex conditions, including hepatitis C; offers a variety of online clinics, trainings, technical assistance, and capacity building.
NPAIHB & CRIHB Joint HCV Resolution
Northwest Portland Area Indian Health Board and California Rural Indian Health Board’s Joint Resolution to create an initiative to eliminate hepatitis C in tribal communities in California, Idaho, Oregon, and Washington.
National Congress of American Indians HCV Resolution #MKE-17-038
NCAI’s adoption and support of NPAIHB’s and CRIHB’s Joint Resolution on hepatitis C elimination.
Indian Country ECHO
Free service for I/T/U clinicians and programs to enhance care delivery for patients with complex conditions, including HCV; offers a variety of online clinics, trainings, technical assistance, and capacity building.
Indian Country ECHO – Technical Assistance and Capacity Building
Free service designed to optimize I/T/U clinical policies, enhance care delivery for patients, and build community capacity to prevent and treat complex medical conditions, including hepatitis C.
Short Films
For Community Members
Hepatitis C: Test, Treat, Cure
For tribal community members about recognizing the symptoms of hepatitis C and the importance of getting treatment.
Hepatitis C is Everyone’s Responsibility
PSA for American Indian and Alaska Native community members about how hep C is everyone’s responsibility.
For Providers & Community Leaders
IHS, Tribal and Urban Clinics are Curing Hepatitis C
Providers can make a difference in patients’ lives through diagnosing hep C early. Learn more about screening and offering patients effective- potentially life-saving – treatment.
Our Mission
The mission of the Enhancing Perspectives in Clinics and Communities (EPCC) Program at the Northwest Portland Area Indian Health Board (NPAIHB) is to build the capacity for Indigenous people, healthcare professionals, traditional knowledge holders, and policymakers to enhance the health and wellness of American Indian and Alaska Native (AI/AN) people and communities.
We believe that it is the role of the Indigenous peoples of Turtle Island to care for our relatives and relations as well as ourselves.
We know we cannot do this alone. That is why we bring together providers, traditional knowledge holders, health advocates, clinic leadership, policymakers, and community members to:
- Develop innovative solutions that advance the health of AI/AN people and communities in positive and affirming ways
- Assist Indigenous people and healthcare professionals in building trusting and compassionate relationships
- Establish innovative and forward thinking clinical and public health policies and practices that rely on Indigenous perspectives, the knowledge of our ancestors, and Western medicine and science
- Build the capacity of leadership across all levels of influence to advance tribal health policy
Our priority is leaving footsteps to help guide the next generation along the path of good health and wellness.
Guided by our leadership, we contribute to clinical and community work in the following priority health issue areas:
- HIV/AIDS
- Hepatitis C
- Substance Use Disorders, including Opioid Use Disorder
- Two Spirit Health and LGBTQ+ Health
- Behavioral Health
- Other emergent health and wellness needs
The EPPC Program directly helps tribes in several ways:
- Technical Assistance and Capacity Building
- Through Indian Country ECHO, we offer free support to IHS, Tribal, and Urban (I/T/U) clinics to optimize their policies and enhance care delivery. Through this service we also offer support to tribal leadership interested in building community capacity to prevent and treat complex medical conditions.
- Quality Improvement
- The EPPC Program collaborates with providers, public health professionals, and administrators to ensure that AI/AN people and communities receive high quality healthcare. Our approach to quality improvement draws on the knowledge of subject matter experts, evidence-based tools, best practices in clinical science, systems theory, Indigenous knowledge, psychology, and other fields of study.
- Patient-Specific Recommendations
- Through a collaboration with the University of California- San Francisco, IHS offers providers practicing at I/T/U facilities on-demand clinical recommendations from experts via the Substance Use Warmline.
- Through Indian Country ECHO, we offer free online ECHO clinics and trainings that provide a platform for providers practicing at I/T/U facilities to receive on-demand clinical recommendations from experts and colleagues across Indian Country.
- Provider and Community Education Campaigns
- EPCC creates evidence-based and community-tested health education campaigns and resources for AI/AN peoples and I/T/U clinicians. These include opioids, HCV, and Two Spirit and LGBTQ+ Health campaigns.
- Our work is generously funded by several entities. EPCC Program initiatives are funded by the Minority HIV/AIDS Fund, Indian Health Service, Substance Abuse and Mental Health Services Administration, and the Office of Minority Health.
For additional information about our program:
Contact Megan Woodbury, Program Manager at the Northwest Portland Area Indian Health Board at mwoodbury@npaihb.org